What are the complications?
Although it is a routine operation, it still is an operation, and each operation can be risky. Complications can be intraoperative (during surgery) and postoperative. The most usual complication is the failure to implant the lens. The patient cannot see and the operation has to be repeated (secondary implantation), but other complications can also occur (bleeding, inflammation, increase of eye pressure). Postoperative complications are longer periods of corneal opacity, wrong artificial lens dioptre, move of the artificial lens and inflammations. The operation is conducted in an operating theatre, under sterile conditions, because inflammation can cause complete blindness. We have to be aware of the fact that a cataract operation can lead to complete blindness (rarely).
What are the degraded conditions for the operation?
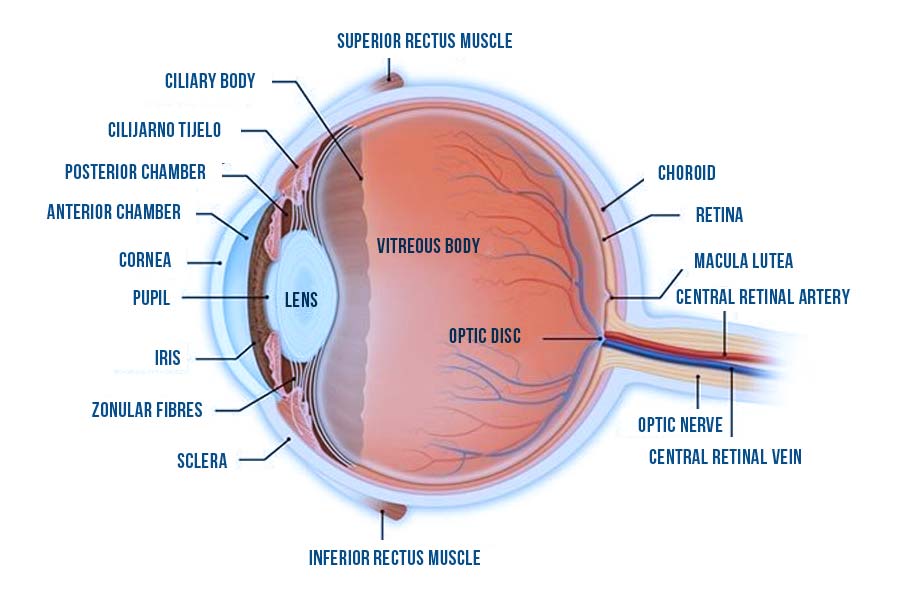
The principle is to open the small bag through a hole, with dilated pupils. The opaque lens is then pounded and aspirated by the ultrasound and an artificial lens is then put into the eye. If you have a ripe cataract (a hard one), high eye pressure, high dioptre, if your pupil does not dilate or you have a relaxed iris, the operation could be harder with higher incidence of complications.
How do I prepare for the operation?
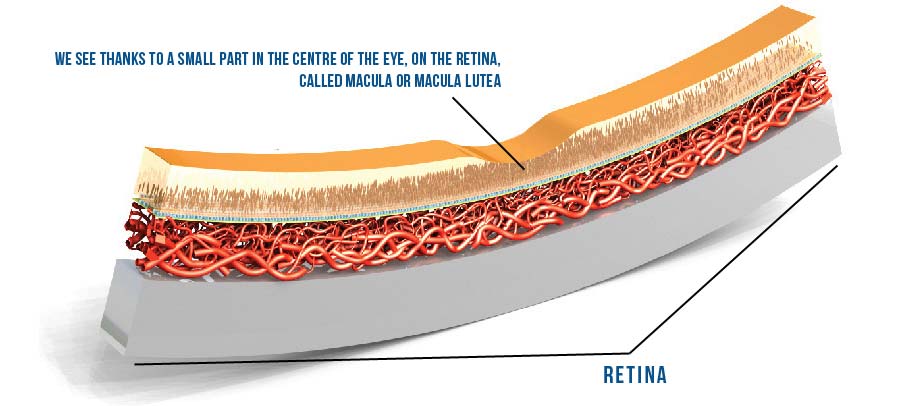
First you have to understand that the cataract causes inconveniences, do not let anyone talk you into the operation. The operation is much easier if you decided to undergo surgery yourself. It is necessary to undergo preoperative examinations (glaucoma, macular degeneration), biometry has to be done (determining the exact dioptre of the lens to be implanted) to achieve the best possible vision without glasses.
On the operation day you will take your everyday therapy and have a light breakfast. In the doctor’s office patients usually get a tranquilizer and eye drops for the pupil dilation are applied.
After the operation you have to keep to the doctor’s advice which will speed up recovery and diminish the possibility of infections. That means that you will have to apply eye drops against infections and inflammations regularly, be at rest and avoid doing hard physical works. In case of any disturbances or doubts on complications, you have to contact your doctor without delay.
The period of recovery lasts from eight to 10 days and after that you can slowly return to your everyday rhythm. After two or three weeks, eyeglasses are ordered if necessary.
What kind of lenses are used in cataract surgery?
These are intraocular artificial lenses which means they are introduced in the eye, in the spot of the removed opaque lens and they are not extracted any more (they are not contact lenses). There are more types of lenses. The basic ones are those which give back the ability to see far objects, while eyeglasses (monofocal) are used for near vision. If the patient has higher cylinders, then lenses with cylinders (toric) are applied, and if patients do not want to wear glasses, then multifocal lenses are applied (with dioptre to be able to see far objects, to work on the computer and to see close objects). It is important to determine the intraocular lens dioptre. This is done by biometry, using a special appliance (each eye has its own dioptre, there are no standard dioptres).
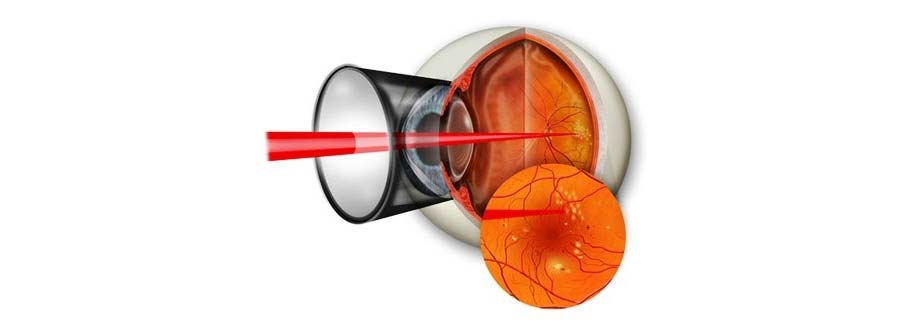
Can cataract reappear?
No, it cannot, but the bag into which the artificial lens has been implanted can become turbid which is solved by laser cleaning of the posterior capsule of the bag turbidity. This is a simple and fast healing method, not an operation. The YAG Laser capsulotomy is done outpatiently.